Want to transform lives with us? Stay in touch and hear about our news, activities and appeals by email!
Changing lives by reducing mental health stigma and discrimination

Ned Carter is a Programme Manager at CBM UK and managed the Time to Change Global programme.
Over the last 15 years CBM and partners have been tackling stigma and discrimination in mental health, and contributing to the global evidence base. Why is this essential? This article looks at an effective stigma reduction approach based on the participation of people with lived experience of mental health conditions.
Stigma in mental health matters
 Through our programmes and partners, people are increasingly participating meaningfully in their communities, accessing dignified quality care and support to meet individual needs, and improving their quality of life and wellbeing.
Through our programmes and partners, people are increasingly participating meaningfully in their communities, accessing dignified quality care and support to meet individual needs, and improving their quality of life and wellbeing.
However, this cannot be achieved when widespread misconceptions and negative beliefs about mental health lead to prejudice and discrimination against people with mental health conditions and psychosocial disabilities.
Stigma could be described as disapproval of someone perceived as “unacceptably different” and distinguished with a mark of social disgrace. People are left feeling shame, guilt and worthlessness, and stigma can cause or exacerbate mental health conditions.
That’s not all. Stigma leading to discriminatory actions can have severe consequences: worse educational outcomes, reduced or denied access to health and social services, exclusion from family and community activities, lower employment and job loss, violence and abuse, poverty, and reduced quality of life.
“The experience of mental illness… the burden to the individual is enough already. For the community to make this even harder is total injustice. We need to change our beliefs. We need to change our thinking.” – Martha, Ghana, volunteer
Given such wide-ranging implications, it’s perhaps not so surprising that people with mental health conditions can describe the barriers and exclusion arising from stigma as worse than the condition itself.
More acceptable knowledge levels, attitudes and behaviours among family members, friends and neighbours, colleagues, service providers, businesses and the public have been shown to bring about practical, positive changes in people’s lives.
But how can this be achieved? It can be hard to change how people think, act and treat others. This is why it is essential to use evidence-based, tried and tested approaches.
“I have been treated very differently because of my mental health problem. I lost my business. I lost everything … In Nigeria people think once you have a mental health problem, you must have done something bad … I’m sharing my story so my child can have a better future. I want him to grow up in a world free from stigma.” – Kabati, Nigeria, volunteer
Effectiveness in stigma reduction
 A systematic review of research by Clay et al (2020) identified core components of effective stigma reduction interventions in low and middle income countries. The authors found that many regions did not report using a “social contact” approach even though there is strong evidence for its effectiveness.
A systematic review of research by Clay et al (2020) identified core components of effective stigma reduction interventions in low and middle income countries. The authors found that many regions did not report using a “social contact” approach even though there is strong evidence for its effectiveness.
Social contact involves conversations between people who have mental health conditions and those who may not. It sounds simple, but it’s powerful.
Among a range of interventions, social contact was described as having the single greatest impact and was therefore recommended for incorporation into anti-stigma projects.
That’s great news for CBM’s mental health programmes.
“The more we talk about it, the more we can reduce the stigma. The more people share their own stories, the more accepting people will be. When these stories hit close to home… then it will be easier for people to accept.” – Tirnom, Nigeria, volunteer
Mental health and stigma programmes
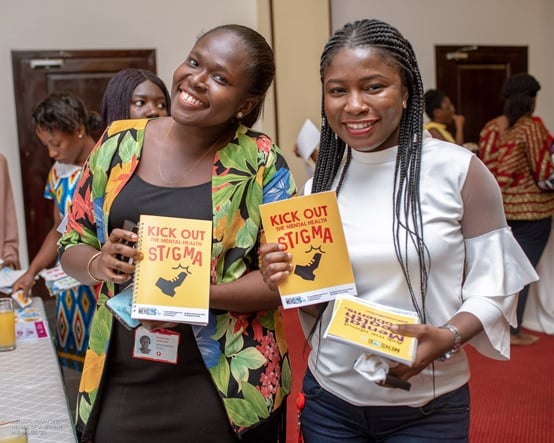
 For example, volunteers in our Time to Change Global programme used social contact to challenge prejudice and change attitudes in their communities.
For example, volunteers in our Time to Change Global programme used social contact to challenge prejudice and change attitudes in their communities.
The quotes in this article are from the volunteers trained and supported to speak out and challenge stigma.
The programme was delivered through a CBM partnership with Mind, Rethink Mental Illness and partners in Nigeria, Ghana, Kenya, Uganda and India, and made possible thanks to funding from Comic Relief and the Department of Health and Social Care.
This was built on years of UK and international social contact research and learning, as well as partner- and volunteer-led delivery and cultural adaptations in each country. Find out more about CBM’s programme (open in new tab) and view the Time to Change toolkit here (open in new tab).
“Generally, when you talk about mental health, people think about madness. That’s not the case … We need to change the whole conversation around mental health.” – Brian, Kenya, volunteer
In Nigeria we are working on a new programme with our partner Mentally Aware Nigeria Initiative (MANI) to deliver activities run by people with lived experience of mental health conditions, such as setting up student advocacy networks that aim to reduce stigma and increase mental health literacy in universities, schools and communities. Learn about CBM’s work in Nigeria here (open in new tab)..
Also in Nigeria, our Neglected Mind Skin Link project is piloting the World Health Organization’s Mental Health of People with Neglected Tropical Diseases guide and investigating care and stigma among people with both mental health conditions and diseases like leprosy and lymphatic filariasis. The guide recommends social contact as a stigma reduction approach. See more about the Mind Skin Link project here (open link in new tab)..
Based on CBM’s experience and wider research, we will be launching a stigma Good Practice Guide. This aims to share our knowledge of delivering effective programmes to reduce stigma in low and middle income countries.
It’s all worth it
So, why do we work on stigma within mental health?
The consequences of stigma and discrimination are all too real. But so are the benefits for people’s lives when we put effective approaches into action.
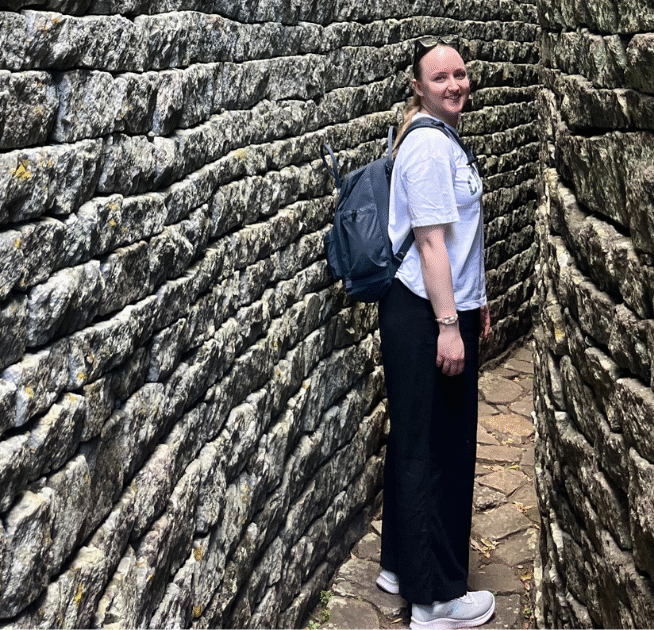
Images – 1st: Volunteers at a social contact event in Ghana. 2nd: Female volunteer at an anti-stigma event in India. 3rd: Volunteers at a social contact event in Ghana. 4th: Volunteers planning a social contact event in India.